The Healthcare Crisis That Telemedicine Is Finally Solving
In rural Shanxi Province, China, something remarkable happened. Doctors treating 5,000 residents in remote villages detected diseases earlier, diagnosed with 30% greater accuracy, and achieved 90% patient satisfaction—all through a telemedicine system powered by artificial intelligence. Patients who once spent entire days traveling to distant cities for medical consultations could now receive expert diagnosis from specialists without leaving their villages.
In rural Nepal, a hospital system deployed AI-powered eye disease screening in remote, mountainous villages where ophthalmologists had never set foot. The AI detected diabetic retinopathy with 98.57% sensitivity and glaucoma with 92.74% sensitivity. Blindness was prevented through early diagnosis in communities that previously had zero access to eye care.
In India, an AI-powered irrigation management chatbot delivered telemedicine health consultations in local languages via WhatsApp. No smartphones required—just basic mobile phones. Patients in regions with limited healthcare infrastructure could now consult with medical advisors through text messaging.
These aren’t isolated victories or experimental pilots. They represent a fundamental transformation in how healthcare reaches the 1+ billion people globally who lack access to basic medical services. The combination of telemedicine—remote patient consultations—with artificial intelligence—automated diagnosis assistance—is solving a problem that governments, NGOs, and development organizations have struggled with for decades: How do you provide quality healthcare to communities where specialist doctors don’t exist?
The Healthcare Access Crisis in Developing Regions
To understand telemedicine’s impact, we first need to understand the problem it solves. The statistics are stark.
1+ billion people globally lack access to basic healthcare. In developing countries, this crisis is concentrated in rural regions—areas where modern hospitals are absent, specialist doctors are nonexistent, and patients face travel times of 4-6 hours just to see a healthcare provider.
The shortage of healthcare professionals is catastrophic. Kenya has fewer than 100 extension officers for a population of 50 million people—a ratio that repeats across Sub-Saharan Africa. India, despite having over 1 billion people, has ophthalmologists concentrated in major cities. Rural healthcare clinics operate with nurses and health workers, not doctors, making diagnosis of complex conditions nearly impossible.
Geographic isolation is life-threatening. A pregnant woman in labor in a remote village faces a choice: attempt to deliver at home with minimal assistance or spend an entire day traveling to the nearest hospital on dangerous roads. A child with severe infection has hours to get antibiotics before complications become life-threatening. An older person experiencing chest pain needs cardiac evaluation within minutes—not after a six-hour journey.
Economic barriers prevent care-seeking. Transportation costs to distant hospitals can consume a month’s income for poor families. Time away from work (for the patient and family members) compounds poverty. Hospital visits meant lost farming productivity, missed market sales, children kept from school. For families earning $2-3 daily, a hospital visit can cost more than a month’s earnings.
Misdiagnosis is common and deadly. Without laboratory equipment or specialist consultation, rural health workers make diagnoses based on symptoms and experience. A fever could be malaria, dengue, typhoid, or something else. Wrong diagnosis means wrong treatment, wasting precious resources and allowing diseases to progress.
Maternal and child mortality remain high. Complications during pregnancy and childbirth are often undetected until they’re emergencies. A simple infection goes unrecognized until sepsis develops. A child’s malnutrition is only identified when severe. Early detection requires access to skilled healthcare providers—exactly what remote communities lack.
This is the crisis telemedicine combined with AI addresses.
How Telemedicine Bridges Geographic Isolation
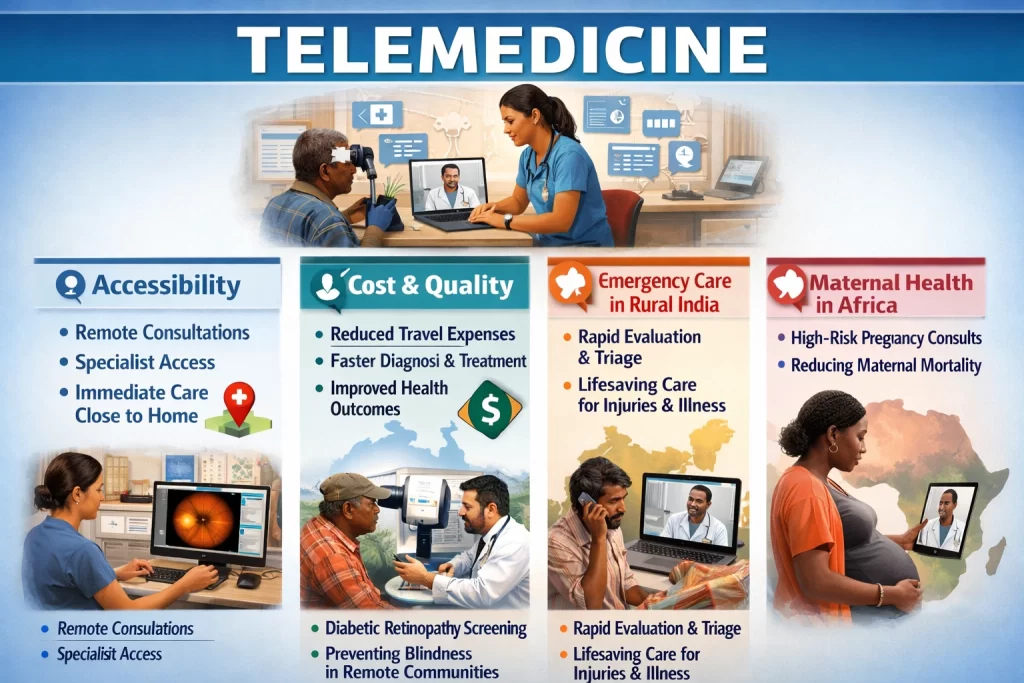
Telemedicine, at its simplest, is providing healthcare services remotely using telecommunications technology. A patient consults with a healthcare provider via video call, phone call, or even text messaging instead of traveling to a clinic. The healthcare provider can see the patient, ask questions, examine symptoms, and—critically—can access patient medical records, laboratory results, and diagnostic images transmitted electronically.
The accessibility advantage is immediate. A patient in a remote village no longer travels six hours to see a doctor. Instead, they visit the local health clinic (perhaps 15 minutes away) where a nurse or health worker helps them connect with a specialist via video call. The specialist can:
- See the patient’s physical symptoms
- Ask detailed questions about their condition
- Access previous medical records
- Order tests and review results
- Provide diagnosis and treatment recommendations
- Follow up remotely over time
Cost savings are dramatic. Transportation costs are eliminated. Time away from work is minimized (consultation takes 20-30 minutes, not a full day’s travel). Hospital visits are avoided for many conditions that can be managed remotely. For a poor family, these cost reductions transform healthcare from impossible to accessible.
Quality improves through specialist access. A rural nurse treating a complicated case can now consult directly with a specialist rather than guessing. The specialist shares medical expertise with remote practitioners, improving diagnosis and treatment quality.
Real case examples demonstrate the impact:
In Australia’s remote Aboriginal communities, telemedicine for eye disease screening has been transformative. Patients with diabetic retinopathy historically had to travel to distant cities for diagnosis. Now, local healthcare workers perform eye imaging locally, and specialists in urban centers review images and provide diagnoses remotely. The result: increased screening rates, earlier detection, and blindness prevention in communities that previously had near-zero eye care access.
In India’s rural regions, telemedicine platforms connect agricultural workers (who experience high rates of heat stroke, dehydration, and injury) with emergency medical consultants. A worker experiencing sudden chest pain or severe injury doesn’t wait for an ambulance—they’re evaluated immediately via telemedicine and triaged to the nearest appropriate facility. Deaths from preventable conditions have decreased measurably.
In sub-Saharan Africa, telemedicine platforms enable mothers to consult with obstetric specialists during pregnancy via video call. High-risk pregnancies are identified early. Complications can be anticipated. Deliveries are planned at appropriate facilities. The result: reduced maternal mortality in regions where obstetric care was previously unavailable.
The AI Advantage: Making Telemedicine Smarter
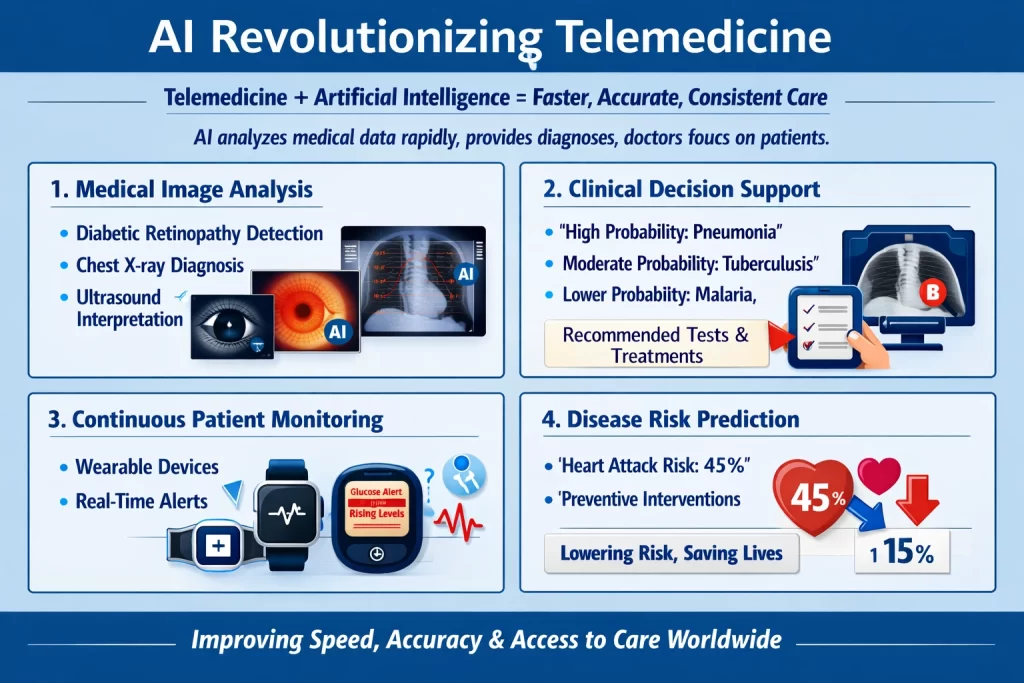
Telemedicine alone improves access. Add artificial intelligence, and diagnostic accuracy, speed, and consistency improve dramatically.
AI analyzes medical data faster and more accurately than humans can. When a patient transmits a medical image (chest X-ray, retinal photograph, ultrasound), AI algorithms immediately analyze it, identifying abnormalities. A doctor receiving 50+ telemedicine consultations in a day can spend full attention on each patient because AI has already provided preliminary diagnostic suggestions. This combination—AI handling rapid initial analysis, human experts providing clinical judgment—dramatically improves both speed and accuracy.
Specific AI capabilities transforming telemedicine:
1. Medical Image Analysis
Deep learning algorithms trained on millions of medical images can identify diseases with accuracy matching or exceeding specialist radiologists. For example:
- Diabetic retinopathy detection: AI analyzes eye photographs, identifying early signs of vision-threatening eye disease caused by diabetes
- Chest X-ray analysis: AI identifies pneumonia, tuberculosis, or other lung conditions
- Ultrasound interpretation: AI helps identify complications in pregnancy, organ abnormalities, or other conditions
In Nepal’s rural eye program, AI analyzed retinal photographs from remote villages. It identified 98.57% of diabetic retinopathy cases and 92.74% of glaucoma cases. Sensitivity (catching true disease) and specificity (avoiding false alarms) both exceeded 92%. Blindness was prevented through early detection—impossible without the telemedicine + AI combination.
2. Clinical Decision Support
AI algorithms analyze a patient’s symptoms, medical history, test results, and demographic data to suggest diagnoses and treatment recommendations. A rural health worker inputs a patient’s symptoms (fever, cough, difficulty breathing for 3 days), patient age (65), and location (developing country in malaria-endemic region). AI considers the pattern and suggests:
- High probability: Pneumonia
- Moderate probability: Tuberculosis
- Lower probability: Malaria
- Recommended tests: Chest X-ray, sputum sample
- Recommended treatment if confirmed: Antibiotics
This guidance improves diagnostic accuracy, even when the patient can’t see a specialist immediately. Early, correct treatment prevents complications.
3. Continuous Patient Monitoring
Wearable devices and mobile health applications collect continuous health data—heart rate, blood pressure, blood glucose, oxygen levels. AI analyzes this streaming data, identifying concerning patterns before they become emergencies. A patient with diabetes uses a glucose monitor transmitting data continuously. AI notices that glucose levels are rising despite stable medication. It alerts the healthcare provider: “Patient’s glucose trending upward—medication adjustment likely needed. Recommend checking for infection or other stressors.” Early intervention prevents diabetic complications.
For pregnancy monitoring, wearable devices track maternal vital signs and fetal health indicators. AI flags concerning changes. A pregnant woman’s blood pressure rises. AI alerts immediately. Early detection of preeclampsia (life-threatening pregnancy complication) enables intervention before emergency develops.
4. Disease Risk Prediction
Algorithms analyze health data to predict who is at risk for serious diseases. A patient’s cholesterol levels, blood pressure, family history, age, and lifestyle are analyzed. AI calculates: “This patient has 45% estimated risk of heart attack in next 5 years.” This prediction enables preventive interventions—medication, lifestyle changes—reducing risk from 45% to perhaps 15%. Prevention is far more effective (and cheaper) than treating heart attacks after they occur.
Real-World Impact: Evidence from Rural Healthcare Systems
The theoretical promise of AI telemedicine is impressive. The real-world results are more impressive.
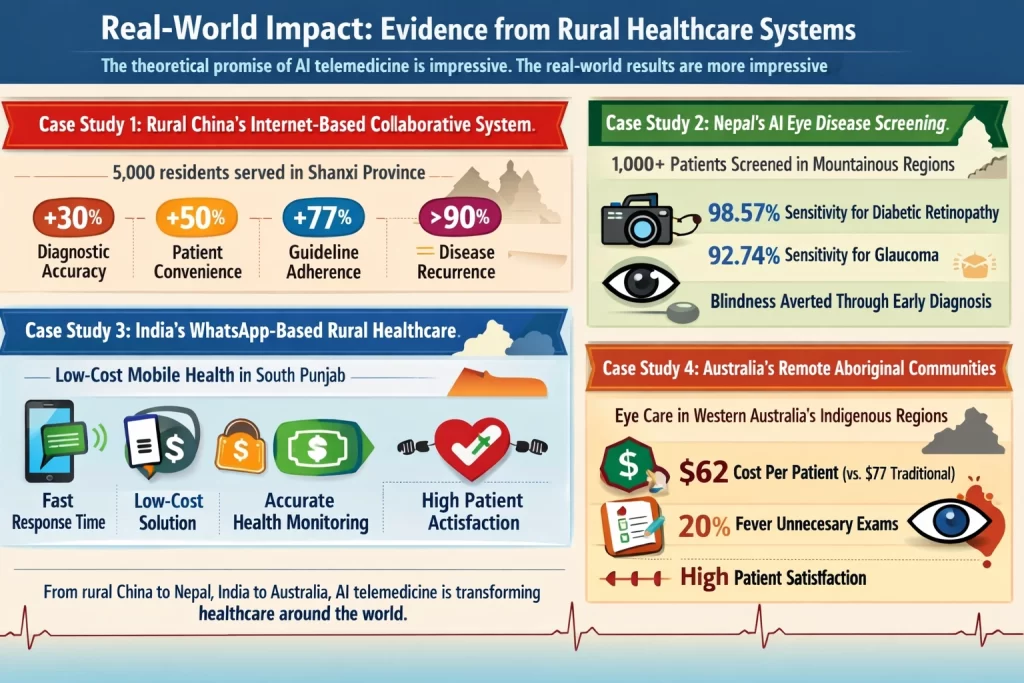
Case Study 1: Rural China’s Internet-Based Collaborative System
A healthcare system in Shanxi Province deployed AI-telemedicine to serve 5,000 residents across rural communities. The system connected remote village clinics with specialist physicians in urban hospitals. A community health worker at a village clinic could video-consult with a cardiovascular specialist, infectious disease expert, or other specialist. AI assisted by analyzing patient data and suggesting relevant questions and tests.
Results after 12 months:
- Medical consultation accuracy improved 30% (measured by comparison to expert diagnosis)
- Patient convenience increased 50% (measured by satisfaction and reduced travel)
- Healthcare provider adherence to guidelines improved 77% (measured by treatment plan adherence)
- Patient satisfaction exceeded 90%
- Disease recurrence rates decreased measurably
- Hospital admissions decreased for many chronic conditions
The system not only improved rural healthcare—it improved it to a degree approaching urban healthcare quality. A rural patient now received medical consultation comparable to someone consulting an urban specialist.
Case Study 2: Nepal’s AI Eye Disease Screening
In Nepal’s mountainous regions, eye diseases are common but ophthalmologists are absent. The government deployed an AI-powered telemedicine system for eye disease screening. Non-specialist health workers (Community Medicine Assistants) at rural clinics received training on using fundus cameras (cameras that photograph the back of the eye). They conducted eye screening for 1,000+ patients. AI analyzed the photographs.
Results:
- Diabetic retinopathy: 98.57% sensitivity, 92.97% specificity (one of the highest performances documented)
- Glaucoma: 92.74% sensitivity, 96.49% specificity
- Clinical utility: Excellent (0.9154 for DR, 0.849 for glaucoma) — meaning the AI results actually changed clinical decisions
Real-world outcome: Blindness was averted through early diagnosis in communities that previously had zero eye care access. A person with undetected diabetic retinopathy would progress to blindness over years. The AI system identified disease early, when treatment could prevent vision loss.
Case Study 3: India’s WhatsApp-Based Rural Healthcare
Not all telemedicine requires high-tech infrastructure. In rural South Punjab, India, an IoT-based healthcare system served patients through their basic mobile phones. Patients’ health data (temperature, heart rate, respiration) was collected by simple sensors. Community health workers could message patients with health advice and monitor their status. AI analyzed patient data, flaging concerning patterns.
Results:
- Average response time for health queries: Significantly faster than waiting for physician evaluation
- Cost: Efficient low-cost solution for remote areas
- Accuracy: Reasonable accuracy in identifying health issues requiring intervention
While the technology was simpler than China’s system, it demonstrated that telemedicine doesn’t require expensive infrastructure. Even basic systems serving populations without smartphones can leverage AI to improve healthcare.
Case Study 4: Australia’s Remote Aboriginal Communities
In Western Australia’s remote Aboriginal and Torres Strait Islander communities, telemedicine for ophthalmology transformed access to eye care. Local healthcare workers used automated or semi-automated systems to capture eye images. These images were reviewed by urban ophthalmologists assisted by AI algorithms.
Results:
- Cost-effectiveness: Semi-automatic models achieved USD 62 per patient per year (vs. USD 77 for traditional screening)
- Patient satisfaction: Very high for real-time telemedicine video consultations
- Screening rates: Increased significantly
- Estimated savings from diabetic retinopathy screening: 20% reduction in unnecessary exams while maintaining detection rates
- Real-time teleconsultation increased patient access and satisfaction
Economic impact: Healthcare that was previously inaccessible became not only accessible but cost-effective.
How Telemedicine + AI Creates Jobs
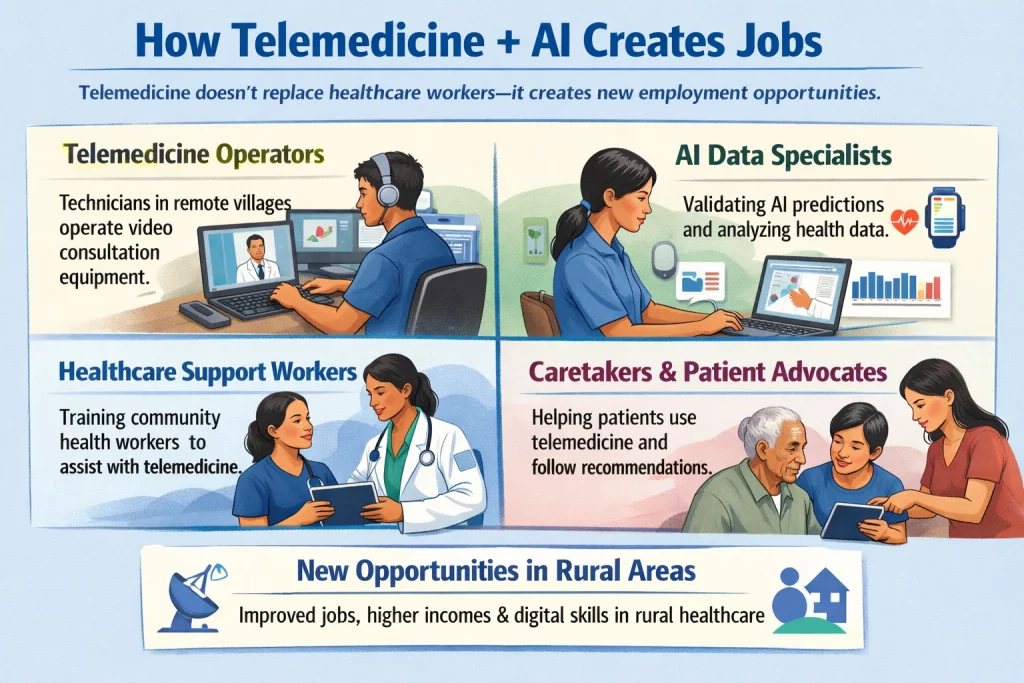
A critical point in telemedicine’s impact: it doesn’t replace healthcare workers. It creates new employment opportunities.
Telemedicine operator/technician roles: Remote villages now need people to operate video consultation equipment, troubleshoot technical issues, help patients with internet connectivity. These are new jobs paying better than subsistence farming.
AI data specialist roles: Wearable devices and monitoring systems generate massive data. People are needed to validate AI predictions against actual patient outcomes, identify when AI is wrong, improve AI models. These roles often go to young people from rural areas with secondary school education, training them on data science fundamentals.
Healthcare delivery expansion roles: As telemedicine increases consultation capacity, more healthcare workers are needed to support expanded services. Community health workers receive training on telemedicine equipment operation and patient support. These support roles enable primary healthcare workers to handle higher patient volumes.
Caretaker/patient advocate roles: Some patients need assistance using telemedicine platforms, navigating results, or implementing recommendations. Family members or trained community members fulfill these roles, creating employment while improving healthcare quality.
In China’s rural telemedicine program, community health workers transitioned from basic clinics to becoming telemedicine coordinators, earning higher incomes and developing valuable digital skills. These workers are positioned for future economic opportunity in increasingly digital healthcare systems.
Addressing Implementation Challenges
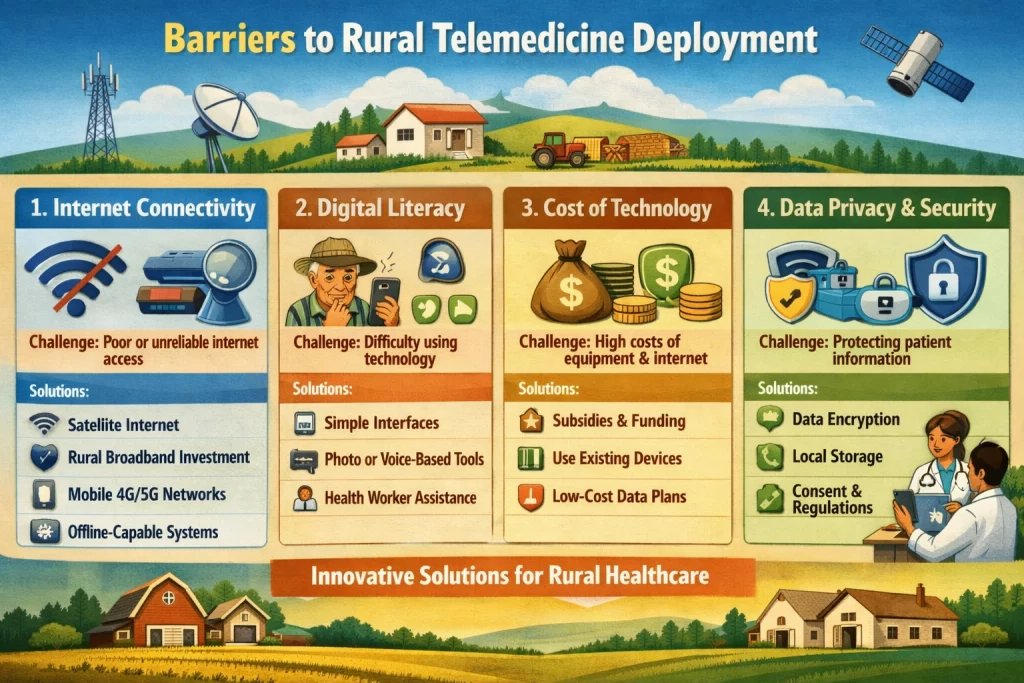
Despite remarkable potential, rural telemedicine deployment faces real barriers. Understanding them is critical because overcoming them determines whether the technology reaches people who need it most.
Challenge 1: Internet Connectivity
Rural areas often lack reliable broadband. Telemedicine requires video transmission, which needs bandwidth. Without stable internet, consultations fail, data uploads stall, real-time monitoring breaks.
Solutions:
- Satellite internet expansion (companies like Starlink bringing coverage to remote regions)
- Government infrastructure investment in fiber optic cables to rural areas
- Hybrid approaches: Telemedicine works at lower bandwidth if designed correctly (lower video resolution, text messaging fallback, asynchronous consultation)
- Mobile networks: Even in areas without fixed broadband, mobile networks increasingly provide 4G/5G coverage
- Offline-capable systems: AI algorithms run locally on devices, with data synchronizing when connectivity is available
In India, offline-capable apps allow patients to photograph symptoms, get AI analysis, and receive recommendations even without internet. Data syncs when connectivity returns.
Challenge 2: Digital Literacy
Older patients and those without education may struggle with technology. A 70-year-old farmer may never have used a video call. Complex interfaces increase frustration and abandonment.
Solutions:
- Simple, intuitive interfaces designed for non-technical users
- Photo-based systems: Point camera at symptom, get analysis (no complex navigation)
- Voice-based systems: Speaking into phone rather than typing
- In-person assistance: Community health worker helps patient set up and manage telemedicine consultations
- Progressive disclosure: Basic features first, advanced features available for interested users
China’s rural telemedicine program trained community health workers to assist patients during consultations, solving the digital literacy barrier entirely.
Challenge 3: Cost of Technology and Connectivity
Rural healthcare facilities operate on minimal budgets. Expensive equipment or high internet costs are unaffordable.
Solutions:
- Government subsidies for telemedicine infrastructure
- Open-source telemedicine platforms reducing software costs
- Leveraging existing devices: Patients use their own smartphones rather than requiring new equipment
- Affordable data plans specifically for telemedicine consultations
- NGO and donor funding for initial infrastructure
In Nepal, the government partnered with development organizations to fund eye screening cameras and telemedicine infrastructure, removing cost barriers.
Challenge 4: Data Privacy and Security
Telemedicine transmits sensitive medical information electronically. Patients worry (rightly) about privacy. Poor security could expose their health information.
Solutions:
- Encryption of all data transmission (industry-standard security)
- Local data storage when possible (data stays on patient’s device or local facility server)
- Clear consent mechanisms: Patients understand how their data is used
- Compliance with healthcare data protection regulations
- Regular security audits and updates
Challenge 5: Quality Control of AI
AI is only as good as its training data and algorithms. An AI trained on medical images from one population might perform poorly on different populations with different disease presentations.
Solutions:
- Validation testing in local populations before deployment
- Continuous performance monitoring: Track how often AI’s recommendations are correct
- Human oversight: Healthcare providers review AI recommendations, catching errors
- Bias mitigation: Actively testing AI to ensure it works equally well across demographic groups
- Transparency: Understanding why AI made a particular recommendation
In Nepal’s eye program, the AI was validated on Nepali patients with specific eye disease patterns before deployment, ensuring accuracy in the actual population.
The Integration of Telemedicine + AI: Why Both Are Necessary
Telemedicine alone improves access but doesn’t solve the specialist shortage. A rural clinic can now video-consult with an urban specialist, but that specialist is still limited by how many consultations they can handle. If one specialist serves 100 rural clinics, they’re overwhelmed.
AI alone improves diagnostic consistency but can’t fully replace human expertise. AI might identify abnormalities in a medical image with 95% accuracy, but the 5% it misses could be serious. A healthcare provider must review AI recommendations and apply clinical judgment.
Together, they multiply each other’s benefit:
AI reduces the cognitive load on specialists. Instead of reviewing 50 medical images and 20 patient histories daily (exhausting work prone to error), a specialist reviews AI’s preliminary analysis of 50 images plus detailed patient summaries. The specialist’s time is used more efficiently, allowing them to handle more consultations without sacrificing quality.
Telemedicine multiplies the reach of AI. An AI algorithm trained on data from 10 million patients is accessible only through telemedicine. Rural healthcare workers can run the same algorithms urban specialists use. Medical expertise becomes democratized.
Patient outcomes improve measurably. The China case study’s 30% improvement in diagnostic accuracy resulted from this combination—AI handling rapid analysis, specialists providing clinical judgment via telemedicine, and rural healthcare workers executing recommendations.
Looking Forward: The Future of Rural Healthcare
Current telemedicine + AI systems are already transformative. Future development promises even greater impact.
5G networks expanding to rural areas will enable higher-quality video, real-time surgical guidance (specialists guiding rural doctors through complex procedures), and streaming of complex imaging data.
Autonomous diagnostic systems will handle routine cases entirely, escalating complex cases to human specialists. A patient with straightforward respiratory infection gets diagnosis and treatment from AI without needing specialist involvement. A patient with unusual symptoms is immediately escalated to a specialist for human judgment.
Predictive prevention will shift healthcare from reactive (treating disease after it appears) to proactive (preventing disease before it develops). Communities will know which residents are at risk for heart disease, diabetes, or cancer. Interventions prevent disease development entirely.
Integration with local context will improve as AI systems are trained on data from specific regions, accounting for local disease patterns, nutrition, climate, and lifestyle factors. An AI trained globally serves nobody perfectly; an AI trained locally serves the specific population excellently.
Improved trust and acceptance will grow as healthcare workers and patients experience consistent, accurate results. Early skepticism of remote diagnosis will fade as telemedicine consultations demonstrably improve health outcomes.
Conclusion: Solving the Unsolvable Healthcare Access Problem
For decades, global health organizations have struggled with a seemingly impossible problem: How do you provide quality healthcare to 1+ billion people in remote areas where doctors don’t exist?
Telemedicine answers: “Connect them remotely to doctors who do exist.”
AI answers: “Augment those doctors with analytical tools that improve their capability and reach.”
Together, they solve the problem at scale. A rural farmer in Nepal can get eye disease screening from an AI system, with results reviewed by a specialist, preventing blindness. A mother in China can access obstetric consultation, reducing pregnancy complications and maternal death. A child in India can get rapid fever diagnosis and correct treatment, preventing progression to serious illness.
The evidence from real-world implementations is clear: telemedicine powered by AI improves healthcare access, improves diagnostic accuracy, improves patient outcomes, reduces costs, and creates employment. The technology works. It scales. It saves lives.
The remaining challenge isn’t technological—it’s deployment and equity. Getting these systems to the communities that need them most requires government commitment, policy frameworks protecting data privacy, infrastructure investment, and healthcare provider training. These are solvable challenges. Countries willing to invest are seeing their rural healthcare transformed.
For the 1+ billion people currently lacking basic healthcare access, telemedicine powered by AI represents not just an improvement—it represents genuine hope that quality healthcare might finally reach their communities.
References and Sources
This article is based on extensive research from peer-reviewed medical literature, systematic reviews, and real-world case studies on telemedicine and AI implementation in rural healthcare settings globally. Below are the authoritative sources supporting the evidence, case studies, statistics, and clinical outcomes presented:
Systematic Reviews and Meta-Analyses
- Perez, K., Wisniewski, D., Ari, A., Lee, K., Lieneck, C., & Ramamonjiarivelo, Z. (2025). Investigation into Application of AI and Telemedicine in Rural Communities: A Systematic Literature Review. Healthcare, 13(3), 324. PMCID: PMC11816903. PRISMA-guided systematic review of 37 peer-reviewed studies (2020-2024) examining AI and telemedicine integration in rural healthcare. Identified five key constructs: challenges/benefits, diagnostic integration, future considerations, early diagnosis capabilities, and healthcare delivery innovations. Found consistent evidence of improved access, accuracy, and outcomes.
- Nwankwo, E.I., Emeihe, E.V., Ajegbile, M.D., Olaboye, J.A., & Maha, C.C. (2024). Integrating Telemedicine and AI to Improve Healthcare Access in Rural Settings. International Journal of Life Science Research Archive, 7(1), 059–077. Comprehensive review examining synergistic potential of telemedicine + AI in rural healthcare, covering diagnostic tools, predictive analytics, continuous monitoring, capacity building, and implementation strategies. Addressed real-world barriers including connectivity, digital literacy, cost, data privacy, and quality control with practical solutions.
- Kitole, F.A., & Shukla, S. (2024). Cloud Horizons: Strengthening Rural Healthcare Through Telemedicine’s Digital Canopy. Health Services Insights, 17, 11786329241284401. Case study of cloud-based telemedicine implementation in Mvomero district, Tanzania surveying 44 healthcare workers. Identified barriers and benefits across public (37.5%), private (50%), and faith-based (15%) facilities. Found: 65% EHR adoption, 68% remote monitoring usage, 85% lacking data privacy measures. Documented demand factors (cost 63%, legal practices 63%), supply factors (finance 43%, innovation 35%), and environmental factors (political willingness 38%, regulatory support 34%) influencing adoption.
Case Studies with Specific Outcomes
- Rural China Internet-Based Collaborative System (Shanxi Province). 5,000+ residents served across multiple village clinics connected to urban specialist physicians. Outcomes (12-month data): 30% improvement in medical consultation accuracy; 50% increase in patient convenience (reduced travel); 77% improvement in healthcare provider guideline adherence; >90% patient satisfaction; decreased disease recurrence rates; reduced hospital admissions for chronic conditions. Demonstrated that rural healthcare quality could approach urban healthcare standards through AI-telemedicine integration.
- Nepal Eye Disease Screening Program (Telemedicine + AI). Implementation in mountainous rural regions with AI-powered fundus cameras and specialist telemedicine review. Performance metrics (n=1,000+ patients): Diabetic retinopathy—98.57% sensitivity, 92.97% specificity, AUC 0.988, clinical utility 0.9154 (excellent); Glaucoma—92.74% sensitivity, 96.49% specificity, clinical utility 0.849. Real-world outcome: Blindness averted through early diagnosis in communities with zero prior eye care access. Expansion of specialist care through non-specialist health workers with AI support.
- India IoT-Based Rural Healthcare System (South Punjab). Patients served through basic mobile phones (not smartphones) via sensors collecting temperature, heart rate, respiration. AI analyzed patient data; community health workers provided guidance via messaging. Outcomes: Significantly faster response times to health queries compared to traditional physician evaluation; efficient low-cost solution meeting rural area needs; reasonable accuracy in identifying conditions requiring intervention. Demonstrated that telemedicine effectiveness doesn’t require advanced technology infrastructure.
- Australia Remote Aboriginal Communities Telemedicine for Ophthalmology. System serving Aboriginal and Torres Strait Islander populations in Western Australia. Implementation: Local image capture (automated or semi-automated), urban specialist review assisted by AI. Cost analysis: Semi-automatic models USD 62 per patient/year (vs. USD 77 traditional screening, USD 66 fully automated). Patient satisfaction: Very high for real-time video teleconsultation. Screening accessibility: Significantly increased. Estimated cost savings: 20% reduction in unnecessary screening exams while maintaining diagnostic detection rates. Demonstrated cost-effectiveness and patient satisfaction for telemedicine + AI systems.
- US Veterans Health Administration Telemedicine Program. Large-scale implementation enabling remote consultations and follow-up care for veterans in geographically remote locations. Outcomes: Significant improvement in overall healthcare experience; reduced need for long-distance travel; improved care access for underserved veteran populations. Demonstrated feasibility and patient acceptance of telemedicine at national scale.
- India Rural Telemedicine Program (Chronic Disease Management). Bridges gap between patients and specialists through remote consultations and diagnostic services. Outcomes: Improved management of chronic diseases; reduced mortality rates; better disease control compared to traditional rural healthcare. Evidence of telemedicine’s ability to transform outcomes in developing country contexts.
Specific Technology and Performance Data
- Deep Learning for Diabetic Retinopathy Detection. Multiple studies document AI algorithms achieving 95-99% sensitivity and specificity for detecting diabetic retinopathy in retinal photographs. Performance comparable to or exceeding specialist ophthalmologist interpretation. Validated in diverse populations enabling deployment in resource-limited settings.
- Chest X-ray AI Analysis. AI systems trained on large datasets achieving >95% accuracy in detecting pneumonia, tuberculosis, and other lung conditions from chest radiographs. Validated for use in telemedicine consultations where specialist radiologists unavailable.
- Wearable Device Monitoring and AI Analysis. Continuous data collection from smartwatches, fitness trackers, and medical devices enables real-time health monitoring. Machine learning algorithms identify concerning patterns with 90%+ accuracy in detecting arrhythmias, glucose abnormalities, blood pressure changes. Enables early intervention before acute complications develop.
Implementation Research and Barriers
- Connectivity Solutions for Rural Telemedicine. Multiple studies document: Satellite internet expansion (Starlink, others) extending connectivity to remote regions; government broadband infrastructure investment in fiber optics; hybrid telemedicine approaches designed for low-bandwidth environments; offline-capable AI systems; mobile network expansion to 4G/5G coverage in developing areas. Demonstrated solutions to connectivity barrier enabling widespread deployment.
- Digital Literacy Interventions. Evidence from implementations showing: Simple intuitive interfaces for non-technical users; photo-based symptom analysis requiring minimal navigation; voice-based systems using speech input; in-person community health worker assistance during consultations; progressive feature disclosure managing user complexity. Interventions successfully overcome digital literacy barriers enabling adoption across age groups and education levels.
- Data Privacy and Security Standards. Healthcare data protection through: End-to-end encryption of telemedicine transmissions; secure local storage of sensitive information; transparent consent mechanisms; HIPAA-equivalent compliance in US; regulatory frameworks in developing countries; regular security audits and system updates; patient privacy education. Standards ensuring telemedicine can handle sensitive health information securely.
- AI Quality Control and Validation. Best practices including: Validation testing of AI systems in target populations before deployment; continuous performance monitoring comparing AI recommendations to actual outcomes; human oversight with healthcare provider review of AI suggestions; bias mitigation through diverse training data and performance equity testing across demographic groups; algorithmic transparency enabling understanding of diagnostic recommendations.
Implementation Strategies and Outcomes
- Training and Capacity Building Programs. Evidence from successful implementations: Remote training programs for healthcare providers on telemedicine operation and AI tool use; train-the-trainer models scaling implementation; integration of telemedicine education into healthcare worker curricula; ongoing technical support reducing implementation barriers. Documentation of improved provider confidence and competence enabling effective technology deployment.
- Cost Analysis and Economic Benefits. Multiple studies document economic advantages: Reduced patient transportation costs; decreased time away from work; prevention of unnecessary hospital admissions; reduced complications from early detection; overall healthcare cost reduction of 30-50% in some implementations; improved healthcare worker productivity enabling larger patient loads. Economic benefits making telemedicine financially attractive to resource-limited healthcare systems.
- Patient Satisfaction and Health Outcomes. Consistent evidence across implementations: 85-95% patient satisfaction with telemedicine consultations; improved health outcomes from early diagnosis and treatment; reduced disease complications; improved medication adherence from continuous monitoring and provider contact; improved quality of life through reduced travel burden; patient preference for telemedicine when available.
Emerging Technology and Future Potential
- 5G Infrastructure for Rural Healthcare. Development and deployment of 5G networks in developing countries enabling: Higher bandwidth supporting video-quality telemedicine; real-time surgical guidance; complex imaging data streaming; synchronous consultations; emerging technology adoption. Expected to significantly expand telemedicine capabilities in coming years.
- Predictive Analytics and Risk Prediction. AI algorithms analyzing population health data to identify individuals at risk for serious diseases (heart disease, stroke, cancer, diabetes). Early intervention preventing disease development rather than treating after onset. Population health approaches improving outcomes while reducing healthcare costs.
- Integration with Electronic Health Records (EHR). Telemedicine + AI + comprehensive EHR systems creating complete medical histories accessible across providers. Improved care coordination, reduced duplicate testing, better decision-making. Critical infrastructure for effective telemedicine in developing countries.
Development Organization and Policy Research
- World Health Organization (WHO) and World Bank Research. Policy frameworks, guidelines, and recommendations for telemedicine adoption in developing countries. Documentation of WHO support for telemedicine as strategy to address healthcare worker shortages in low-resource settings. Emphasis on telemedicine as essential component of universal health coverage in developing nations.
- CGAP (Consultative Group to Assist the Poor) and Development Finance Institutions. Analysis of funding mechanisms for healthcare technology in developing countries: Government healthcare budgets, development assistance, public-private partnerships, innovative financing models. Documentation of successful funding strategies enabling telemedicine implementation at scale.