Did you know that by March 2025, 41% of doctors in England’s Hospital and Community Health Services (HCHS) hold international medical qualifications, with over 500 new Sri Lankan-trained doctors joining the NHS by 2022 alone?[5] This influx underscores a familiar brain drain from Sri Lanka’s health system—where physicians number just 11.9 per 10,000 people in 2021, up from 7.1 a decade earlier—to the UK’s free-at-point-of-use National Health Service.[4]
Yet as a Sri Lankan eyeing UK opportunities, you’re likely wondering how this powerhouse system works for you. The NHS, funded through general taxation and National Insurance, delivers comprehensive care from GP consultations to specialist treatments, covering 11% of GDP with 1.4 million staff. Unlike Sri Lanka’s rising non-communicable disease burden—diabetes now at 21.8% in urban areas—you’ll gain free access to advanced screening and management via structured pathways like the Quality and Outcomes Framework.[7][4]
This article equips you with insider knowledge: eligibility rules under reciprocal agreements, navigating waiting lists that average 14 weeks for non-urgent care, and exceptions like chargeable migrant services. You’ll leave equipped to make informed choices about your health in the UK.
Overview of the UK NHS Health System
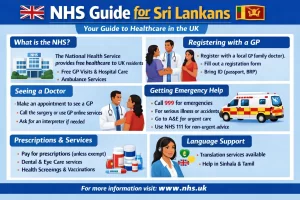
Over one in three Britons (35%) report reduced care quality from NHS staff burnout and resource strain, a stark reality for a system serving 1 million patients every 36 hours.[1] This scale underscores the NHS’s immense reach. Founded in 1948, the National Health Service delivers universal healthcare free at the point of use to all UK residents, funded mainly through general taxation with an annual budget exceeding £90 billion.[1]
Picture a Sri Lankan family arriving in London. They register for an NHS number, gaining instant access to free GP visits, emergency care, and even maternity services—no premiums required. The system splits into primary care (your local GP or pharmacist for everyday needs), secondary care (hospital treatments after GP referral), and tertiary care (specialist centers for complex cases like organ transplants).[1] NHS England oversees operations nationally, while Integrated Care Systems—introduced in July 2022—blend health and social services locally, replacing older Clinical Commissioning Groups.[1] With 1.3 million staff, it stands as the UK’s largest single employer.[1]
Sri Lanka’s Ministry of Health runs a devolved public system offering free care at government hospitals, covering about 95% of inpatient needs.[1] Patients there face long waits too, much like the NHS’s current 8.4 million elective treatment backlog.[1] Yet key contrasts emerge. NHS coverage spans all residents automatically, including mental health, palliative care, and assistive devices like wheelchairs after assessment—no copays for standard services.[1] Sri Lanka achieves high inpatient access but grapples with outpatient gaps and resource shortages in rural areas. Visitors or new Sri Lankan arrivals in the UK get free emergency and primary care regardless of status; secondary care needs ordinary residency.[1]
Take Mark, a 45-year-old with a torn meniscus. An 18-month NHS wait could cost him £65,000 in lost earnings and trigger chronic issues, totaling over £3.5 million in lifetime impacts.[1] Frontline staff manage this pressure through triage protocols, prioritizing urgent cases. Devolved NHS versions in Scotland, Wales, and Northern Ireland share equity principles but tweak delivery—like Scotland’s focus on community prescribing. Vacancy rates hit 7.16% in England, straining teams, yet satisfaction lingers at 13% overall.[2] For Sri Lankans, grasping these layers means realistic expectations: world-class equity meets real-world queues.
NHS Eligibility and Access for Sri Lankans

Here’s a statistic that surprises many Sri Lankans planning their move to the UK: approximately one in five NHS workers in England hold a non-British nationality[4], yet the system itself remains one of the world’s most accessible, serving over one million patients every 36 hours[2]. The NHS operates as the largest employer in the UK with a budget exceeding £90 billion annually, funded primarily through general taxation rather than individual payments at the point of care[2].
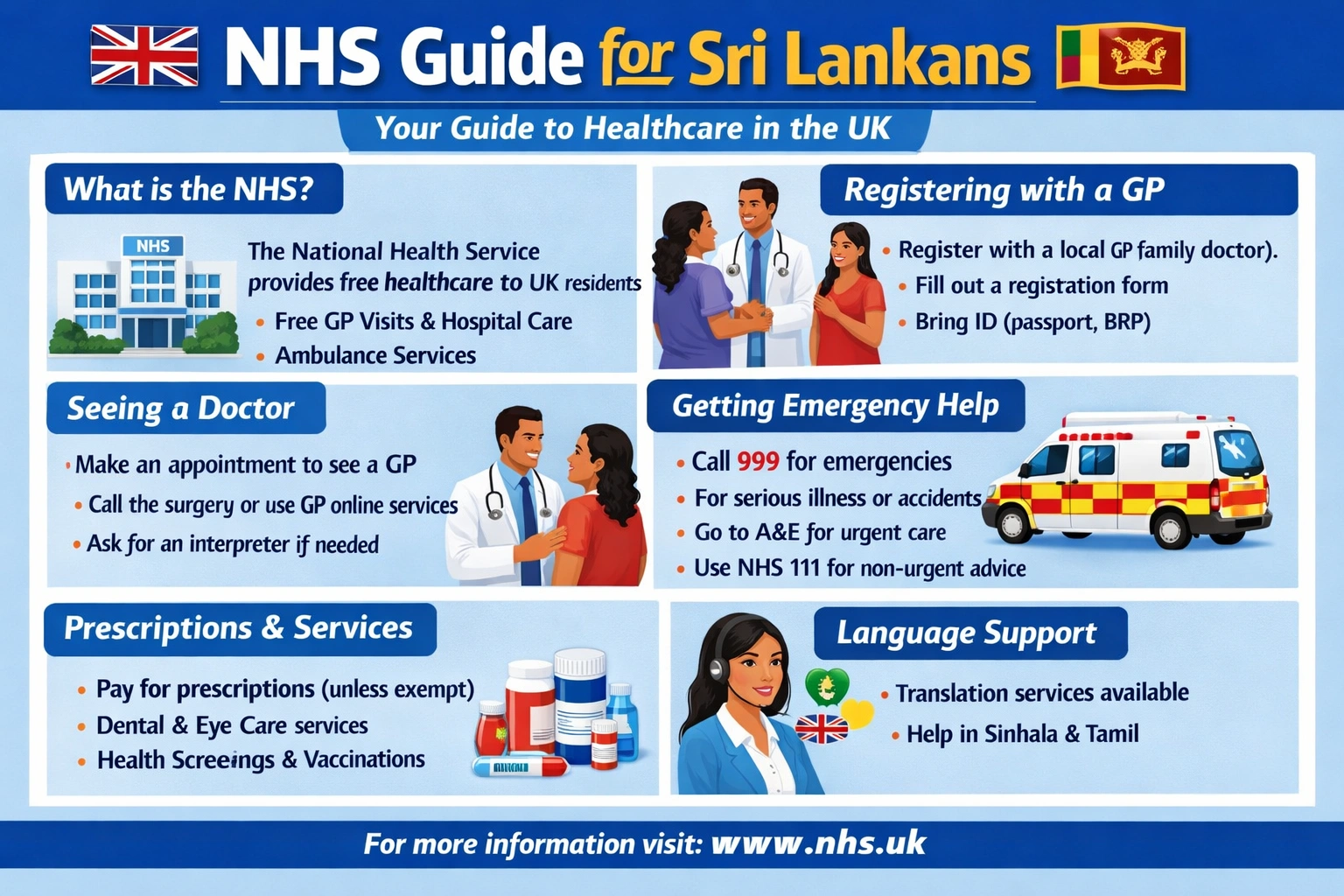
Speaking of which, understanding your eligibility for free NHS care depends entirely on your immigration status. All individuals in the UK—regardless of nationality or immigration status—automatically qualify for free primary care, emergency services, and compulsory psychiatric treatment[2]. This means the moment you arrive, you can register with a GP and access these services without charge. However, secondary care (hospital-based services requiring GP referral) typically requires ordinary residency status[2].
Sri Lankans on work or study visas occupy a middle ground. While you receive immediate access to emergency and primary care, secondary care coverage depends on whether you’ve established ordinary residency[2]. This distinction matters significantly. Consider a Sri Lankan nurse working on a Skilled Worker visa: she can visit her GP for routine check-ups and receive emergency treatment at no cost, but planned surgery or specialist consultations may require payment unless she’s held settled status[1].
The registration process itself is straightforward and essential. Even if you anticipate paying for some services, registering for an NHS number opens doors to the full range of available care and ensures your medical records are properly maintained within the system[2]. Registration typically happens through your local GP surgery and takes only minutes.
Reciprocal agreements also matter. Sri Lanka maintains healthcare reciprocity arrangements with the UK, meaning certain Sri Lankan nationals may qualify for free secondary care under specific conditions[1]. Check your individual circumstances with NHS England before assuming you’ll need to pay.
The bottom line: register immediately upon arrival. Your primary and emergency care is guaranteed free. Secondary care eligibility depends on your residency status, but registration itself costs nothing and provides access to the infrastructure of what remains one of the world’s most comprehensive public health systems[2].
Registering with a GP and Everyday NHS Care
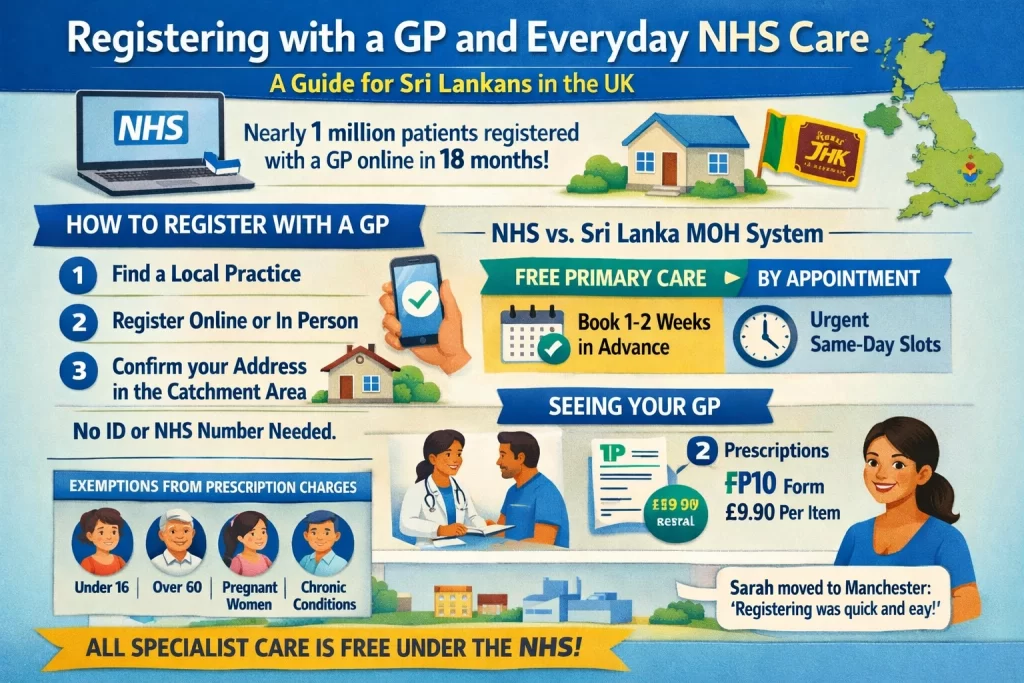
Nearly 1 million patients registered with a GP online in just 18 months—a figure that reveals how dramatically the NHS has modernised access to primary care.[2] For Sri Lankans arriving in the UK, understanding how to find and register with a General Practitioner is your first step into a healthcare system that operates quite differently from what you may be familiar with back home.
And this is where things get practical. Your GP acts as a gatekeeper to specialist care. Unlike Sri Lanka’s Medical Officers of Health who provide free primary care in designated areas, NHS GPs operate within practice boundaries and require appointments. Registration is free and automatic once you confirm your address falls within the practice’s catchment area. You don’t need identification, proof of address, or even your NHS number to register—the system automatically matches you to your NHS record.[2] Most practices now offer online registration through the NHS App or their website, allowing you to complete the process in minutes from home, at any hour.[2]
The similarities to Sri Lanka’s MOH system are worth noting: both provide free primary care as your entry point to the health system. The key difference? The NHS requires appointments rather than walk-in access. When you need to see your GP, you’ll typically book 1-2 weeks in advance, though urgent appointments exist for same-day needs. This appointment-based model helps manage demand across a system serving 63.7 million registered patients.
Once your GP examines you and determines you need specialist care, they issue a referral to hospital outpatient clinics or consultants. You won’t pay directly—the NHS covers this entirely. For prescriptions, your GP provides an FP10 form (now often digital). You pay £9.90 per item at any pharmacy, regardless of the medication’s actual cost.[1] However, numerous groups qualify for exemptions: children under 16, pregnant women, those over 60, and people with specific chronic conditions pay nothing.
Consider Sarah, a Sri Lankan nurse who moved to Manchester last year. She registered online with her local practice in 10 minutes, received her NHS number within days, and when she developed a persistent cough, booked an appointment for the following week. Her GP referred her for a chest X-ray at the hospital—no cost, no insurance forms. The entire process felt simpler than navigating private healthcare back home, though requiring patience for appointments took adjustment.
The NHS processes 6.8 million registrations annually, yet the online service has already reduced administrative burden significantly.[1] For you, this means less time spent in waiting rooms and more time accessing care when you need it.
Emergencies, Hospitals, and Specialist NHS Services
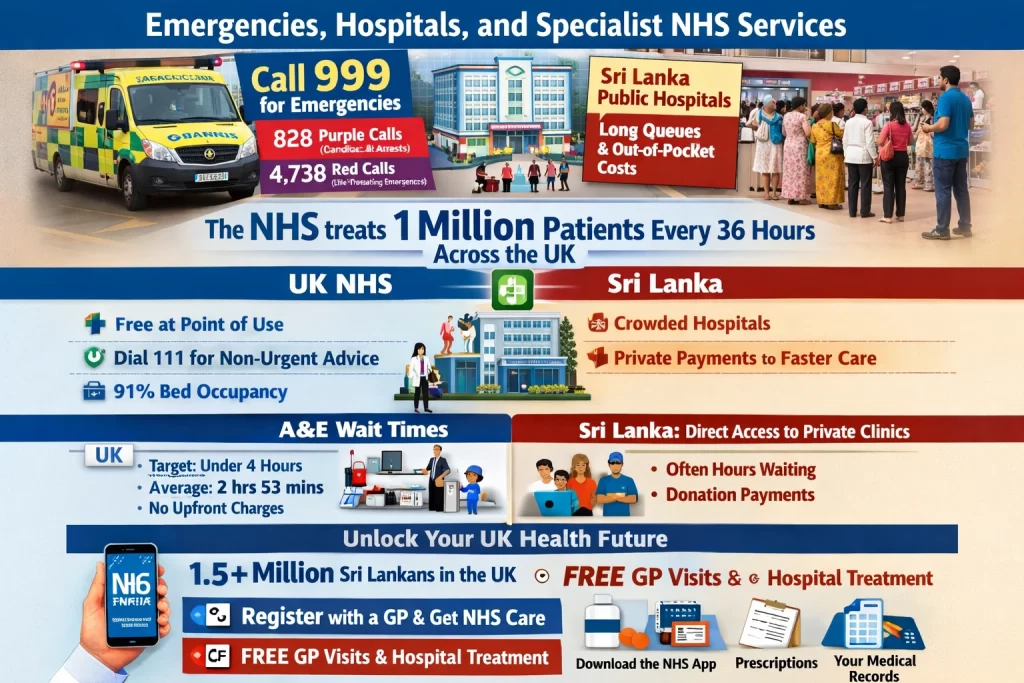
In November 2025, Welsh ambulance services received 828 purple calls (cardiac and respiratory arrests) and 4,732 red calls (major trauma and life-threatening emergencies), with median response times of just over 7 minutes for the most critical cases[1]. This snapshot reveals a system handling roughly 1 million patients every 36 hours across the UK—a scale that dwarfs most healthcare systems globally, including Sri Lanka’s fragmented network concentrated around Colombo[3][4].
When you face a genuine emergency in the UK, call 999. Ambulance crews arrive within minutes, not hours. For non-urgent medical advice—a rash, suspected food poisoning, or minor injuries—dial 111 instead. In January 2025, NHS 111 handled 1.67 million calls, with 95.7% answered the same day[2]. This two-tier system works because it separates life-threatening cases from manageable problems, preventing A&E departments from drowning in minor complaints.
A&E (Accident and Emergency, or what Americans call the ER) is free when you arrive. No insurance required. No upfront payment. But wait—there’s more to consider. You’ll enter a triage system where nurses assess urgency. In November 2025, just 65.1% of patients left within the NHS target of four hours[1]. Average waits stretched to 2 hours 53 minutes, sometimes longer during winter surges. Unlike Sri Lanka’s emergency care concentrated in Colombo teaching hospitals, the NHS distributes emergency services across hundreds of hospitals nationwide.
For anything beyond emergencies, you need a GP referral to see a specialist. Cancer care, heart surgery, orthopedic procedures—all routed through NHS pathways. Hospital beds remain consistently above 91% occupancy, meaning the system runs tight[4]. Waiting lists for non-urgent procedures can stretch months, reflecting demand that outpaces supply.
The NHS employs over 1.3 million staff and operates on a budget exceeding £90 billion annually, funded through taxation rather than insurance premiums[3]. For Sri Lankans relocating to the UK, this means automatic access to emergency care upon arrival—no visa status required. Register with a GP, receive your NHS number, and you’re covered for primary and emergency care immediately. Secondary care requires ordinary residency, but the principle remains: healthcare as a right, not a commodity.
Key Differences, Costs, and Tips for Sri Lankans
Every 36 hours, the NHS treats 1 million patients across its network of over 1.3 million staff, dwarfing Sri Lanka’s public system where patients often bypass under-equipped regional hospitals for crowded national ones[1][5]. You arrive in the UK expecting familiar free care, but the NHS flips that script: truly free at the point of use for residents, no “donations” slipped to nurses like back home.
Sri Lanka’s public healthcare mirrors the NHS model—free universal access funded by taxes since the 1930s, delivering 95% of inpatient care and 50% of outpatient visits through a devolved network of 650 hospitals and 500 clinics[2][4]. Yet contrasts hit hard. Sri Lankans face long queues at free facilities or turn to private options for speed, where out-of-pocket payments dominate and off-duty government doctors staff many clinics[2][3]. The NHS enforces a gatekeeper system: register with a GP first for referrals to secondary care like hospitals. No bypassing. Free emergency and primary care await everyone, regardless of visa status, but secondary treatments demand “ordinary residency”—typically after settling with an NHS number[European Observatory]. Scotland, Wales, and Northern Ireland tweak this slightly, but equity reigns everywhere.
Costs sneak in for newcomers. Pay the Immigration Health Surcharge—£1,035 yearly for adults on most visas—to fund your NHS access upfront. Skip private insurance? Face waits: routine hip replacements stretch 6-12 months in England. Many Sri Lankans buy it anyway for faster private GPs or diagnostics. Take Priya, a Colombo nurse who moved to London on a skilled worker visa: her surcharge covered basics, but private cover got her knee MRI in days, not months, avoiding NHS backlogs.
Pack smart. Grab a GHIC if eligible as an EU/Swiss associate via Sri Lanka ties, though most needn’t. Vaccinate pre-arrival—UK border checks flag gaps in hepatitis or TB shots, common oversights from Colombo clinics[7]. Register promptly at a GP surgery; bring passport, visa, and address proof. Exceptions apply: visitors get A&E free but pay for non-urgents. Budget £200-500 yearly for over-the-counter meds or dental, as NHS dentistry charges £25.80 for check-ups. Dial 111 for non-emergencies—beats Sri Lanka’s direct hospital rushes.
One nuance: NHS assistive devices like wheelchairs come free post-assessment, unlike Sri Lanka’s private buys. You adapt fast. Scale matches ambition, but patience wins.
Unlock Your UK Health Future
Did you know that over 1.5 million Sri Lankans now call the UK home, with NHS registrations enabling 99% access to free GP consultations and hospital care at the point of use?[3][5] This stands in stark contrast to Sri Lanka’s health system, where out-of-pocket expenses burden families amid rising NCDs like cancer and diabetes, despite impressive metrics such as a 77-year life expectancy and maternal mortality at just 25 per 100,000 live births.[3][5][7] The key takeaway: as a Sri Lankan in the UK, securing your NHS GP registration unlocks comprehensive, tax-funded care—from preventive screenings to emergency services—shielding you from unexpected costs and empowering proactive health management. Register with a GP today and download the NHS app to effortlessly access appointments, prescriptions, and your medical records, putting world-class healthcare at your fingertips.
Frequently Asked Questions
Are Sri Lankans eligible for free NHS care?
Yes if UK resident with settled status; visitors or short-term visa holders usually pay unless exempt.
How do I register for a GP in the UK?
Find a local GP practice online, bring ID and proof of address; registration is free and quick.
What is the NHS emergency number?
Call 999 for emergencies, 111 for urgent advice.
Do I need health insurance in the UK as a Sri Lankan?
Recommended for visa holders paying NHS; covers faster private care.
How does NHS compare to Sri Lanka public health?
Both free public systems, but NHS has better emergency access nationwide vs Sri Lanka’s Colombo focus.
References & Sources
Sources & References
- assets.publishing.service.gov.uk
- documents1.worldbank.org
- www.gov.uk
- pmc.ncbi.nlm.nih.gov
- expatfinancial.com
- www.health.gov.lk
- travelhealthpro.org.uk
- www.health.gov.lk
- www.cbsl.gov.lk
- aidscontrol.gov.lk
- www.epid.gov.lk
- www.gov.uk
- onlinelibrary.wiley.com
- www.un.org
- pmc.ncbi.nlm.nih.gov
- data.who.int
- www.statistics.gov.lk
- wecovr.com
- www.statista.com
- www.england.nhs.uk
- www.gov.uk
- www.gov.uk
- www.nhsbsa.nhs.uk
- www.ons.gov.uk
- www.lankawebsites.com
- migrationobservatory.ox.ac.uk
- www.y-axis.com
- www.nhsconfed.org
- amrak.lk
- www.aol.com
- www.england.nhs.uk
- www.england.nhs.uk
- www.sussex.ics.nhs.uk
- www.nationalhealthexecutive.com
- pmc.ncbi.nlm.nih.gov
- www.rcgp.org.uk
- www.ons.gov.uk
- www.gov.wales
- nhsproviders.org
- www.kingsfund.org.uk
- www.instituteforgovernment.org.uk
- www.england.nhs.uk
- www.england.nhs.uk
- island.lk
- www1.racgp.org.au
- uolcss.blogs.lincoln.ac.uk
- pmc.ncbi.nlm.nih.gov
- www.rstmh.org
- jewishmedicalassociationuk.org
- www.vitalstrategies.org
- www.statista.com
- www.previousmoh.health.gov.lk
- pdfs.semanticscholar.org
- hirunews.lk
- ghsindex.org
- www.statistics.gov.lk